Abstract
Summary
This study demonstrated an impaired biomaterial-mediated bone regeneration in a critical sized calvarial defect established within an ovariectomized rat model. Histological and microtomographic evidences were supported by an impaired osteoblastic gene expression and altered expression of estrogen receptors and adipogenic markers.
Introduction
This work aims to address the bone regeneration process in the ovariectomized rat model, by assessing a calvarial critical size defect implanted with a biocompatible bovine bone mineral graft.
Methods
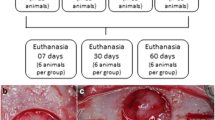
Animals were randomly divided into two groups: Ovx (bilateral ovariectomy) and Sham (control surgery). Following 8 weeks, all animals were submitted to a surgical bicortical craniotomy (5-mm circular critical size defect), which was filled with a biocompatible mineral graft. Animals were euthanized at 1, 3, and 6 months following graft implantation (n = 10), and results on the orthotopic bone regeneration process were blindly evaluated by radiographic, microtomographic, histological, histomorphometric, and gene expression techniques.
Results
In the attained model, in both Sham and Ovx groups, the bone regenerative process was found to occur in a slow-paced manner. Likewise, a qualitative evaluation of the microtomographic and histological analysis, as well as quantitative data from histomorphometric indexes, revealed reduced bone regeneration in Ovx animals, at the assayed time points. Significant differences were attained at the 3 and 6 months. Gene expression analysis revealed a reduced expression of osteoblastic-related genes and an altered expression of estrogen receptors and adipogenic markers, within the regenerating bone of Ovx animals.
Conclusions
Due to the similarities between the osteoporotic animal model and the human condition of postmenopausal osteoporosis, it might be relevant to consider the potential clinical implication of the osteoporotic condition in the biomaterial-mediated bone tissue healing/regeneration process.




Similar content being viewed by others
References
Mikosch P (2012) Osteoporosis: pathophysiology and clinical aspects. In: Pietschmann P (ed) Principles of osteoimmunology. Springer, Vienna, pp 137–167
NIH Consensus Development Panel on Osteoporosis Prevention (2001) Osteoporosis prevention, diagnosis, and therapy. J Am Med Assoc 285:785–795
Poole K, Treece G, Ridgway G, Mayhew P, Borggrefe J, Gee A (2011) Targeted regeneration of bone in the osteoporotic human femur. PLoS One 14:e16190
Leppänen O, Sievänen H, Jokihaara J, Pajamäki I, Kannus P, Järvinen T (2008) Pathogenesis of age-related osteoporosis: impaired mechano-responsiveness of bone is not the culprit. PLoS One 2:e2540
Khosla S, Westendorf JJ, Oursler MJ (2008) Building bone to reverse osteoporosis and repair fractures. J Clin Invest 118:421–428
Dominguez L, Scalisi R, Barbagallo M (2010) Therapeutic options in osteoporosis. Acta Biomed 81(Suppl 1):55–65
Fini M, Nicoli Aldini N, Gandolfi MG et al (1997) Biomaterials for orthopedic surgery in osteoporotic bone: a comparative study in osteopenic rats. Int J Artif Organs 20:291–297
Hayashi K, Uenoyama K, Matsuguchi N, Nakagawa S, Sugioka Y (1989) The affinity of bone to hydroxyapatite and alumina in experimentally induced osteoporosis. J Arthroplasty 4:257–262
Teofilo JM, Brentegani LG, Lamano-Carvalho TL (2004) Bone healing in osteoporotic female rats following intra-alveolar grafting of bioactive glass. Arch Oral Biol 49:755–762
Fini M, Giavaresi G, Aldini N et al (2000) The effect of osteopenia on the osteointegration of different biomaterials: histomorphometric study in rats. J Mater Sci Mater Med 11:579–585
Okazaki A, Koshino T, Saito T, Takagi T (2000) Osseous tissue reaction around hydroxyapatite block implanted into proximal metaphysis of tibia of rat with collagen-induced arthritis. Biomaterials 21:483–487
Tami A, Leitner M, Baucke M, Mueller T, van Lenthe G, Müller R, Ito K (2009) Hydroxyapatite particles maintain peri-implant bone mantle during osseointegration in osteoporotic bone. Bone 45:1117–1124
Thomsen J, Laib A, Koller B, Prohaska S, Mosekilde L, Gowin W (2005) Stereological measures of trabecular bone structure: comparison of 3D micro computed tomography with 2D histological sections in human proximal tibial bone biopsies. J Microsc 218:171–179
Komlev V, Mastrogiacomo M, Pereira R, Peyrin F, Rustichelli F, Cancedda R (2010) Biodegradation of porous calcium phosphate scaffolds in an ectopic bone formation model studied by X-ray computed microtomograph. Eur Cell Mater 19:136–146
Luvizuto E, Tangl S, Zanoni G, Okamoto T, Sonoda C, Gruber R, Okamoto R (2011) The effect of BMP-2 on the osteoconductive properties of β-tricalcium phosphate in rat calvaria defects. Biomaterials 32:3855–3861
Hollinger JO, Kleinschmidt JC (1990) The critical size defect as an experimental model to test bone repair materials. J Craniofac Surg 1:60–68
Gomes P, Fernandes M (2011) Rodent models in bone-related research: the relevance of calvarial defects in the assessment of bone regeneration strategies. Lab Anim 45:14–24
Surve V, Andersson N, Lehto-Axtelius D, Håkanson R (2001) Comparison of osteopenia after gastrectomy, ovariectomy and prednisolone treatment in the young female rat. Acta Orthop Scand 72:525–532
Hara T, Sato T, Oka M, Mori S, Shirai H (2001) Effects of ovariectomy and/or dietary calcium deficiency on bone dynamics in the rat hard palate, mandible and proximal tibia. Arch Oral Biol 46:443–451
Rawlinson S, Boyde A, Davis G, Howell P, Hughes F, Kingsmill V (2008) Ovariectomy vs. hypofunction: their effects on rat mandibular bone. J Dent Res 88:615–620
Egermann M, Goldhahn J, Schneider E (2005) Animal models for fracture treatment in osteoporosis. Osteoporos Int 16:S129–S138
Asarian L, Geary N (2002) Cyclic estradiol treatment normalizes body weight and restores physiological patterns of spontaneous feeding and sexual receptivity in ovariectomized rats. Horm Behav 42:461–471
Brown L, Clegg D (2010) Central effects of estradiol in the regulation of food intake, body weight, and adiposity. J Steroid Biochem Mol Biol 122:65–73
Turner RT, Maran A, Lotinun S, Hefferan T, Evans GL, Zhang M, Sibonga JD (2001) Animal models for osteoporosis. Rev Endocr Metab Disord 2:117–127
Lelovas P, Xanthos T, Thoma S, Lyritis G, Dontas I (2008) The laboratory rat as an animal model for osteoporosis research. Comp Med 58:424–430
Durão S, Gomes P, Silva-Marques J, Fonseca H, Carvalho J, Duarte J, Fernandes M (2012) Bone regeneration in osteoporotic conditions: healing of subcritical-size calvarial defects in the ovariectomized rat. Int J Oral Maxillofac Implants 27:1400–1408
Bosch C, Melsen B, Vargervik K (1998) Importance of the critical-size bone defect in testing bone-regenerating materials. J Craniofac Surg 9:310–316
Hayashi K, Uenoyama K, Mashima T, Sugioka Y (1994) Remodelling of bone around hydroxyapatite and titanium in experimental osteoporosis. Biomaterials 15:11–16
Fuegl A, Tangl S, Keibl C, Watzek G, Redl H, Gruber R (2011) The impact of ovariectomy and hyperglycemia on graft consolidation in rat calvaria. Clin Oral Implants Res 22:524–529
Iwashita Y, Yamamuro T, Kasai R, Kitsugi T, Nakamura T, Okumura H, Kokubo T (1992) Osteoconduction of bioceramics in normal and osteopenic rats: comparison between bioactive and bioinert ceramics. J Appl Biomater 3:259–268
Ribeiro D, Figueira L, Issa J, Vecina C, Dias F, Cunha M (2012) Study of the osteoconductive capacity of hydroxyapatite implanted into the femur of ovariectomized rats. Microsc Res Tech 75:133–137
Rodríguez JP, Garat S, Gajardo H, Pino AM, Seitz G (1999) Abnormal osteogenesis in osteoporotic patients is reflected by altered mesenchymal stem cells dynamics. J Cell Biochem 75:414–423
Carbonare LD, Valenti MT, Zanatta M, Donatelli L, Lo Cascio V (2009) Circulating mesenchymal stem cells with abnormal osteogenic differentiation in patients with osteoporosis. Arthritis Rheum 60:3356–3365
Benisch P, Schilling T, Klein-Hitpass L et al (2012) The transcriptional profile of mesenchymal stem cell populations in primary osteoporosis is distinct and shows overexpression of osteogenic inhibitors. PLoS One 7:e45142
Zaman G, Jessop HL, Muzylak M, De Souza RL, Pitsillides AA, Price JS, Lanyon LL (2006) Osteocytes use estrogen receptor α to respond to strain but their ERα content is regulated by estrogen. J Bone Miner Res 21:1297–1306
He Y-X, Zhang G, Pan X-H, Liu Z, Zheng L-Z, Chan C-W, Lee K-M, Cao Y-P, Li G, Wei L (2011) Impaired bone healing pattern in mice with ovariectomy-induced osteoporosis: a drill-hole defect model. Bone 48:1388–1400
Chagin A, Lindberg MK, Andersson N, Moverare S, Gustafsson JÅ, Sävendahl L, Ohlsson C (2004) Estrogen receptor-β inhibits skeletal growth and has the capacity to mediate growth plate fusion in female mice. J Bone Miner Res 19:72–77
Ke HZ (2005) In vivo characterization of skeletal phenotype of genetically modified mice. J Bone Miner Metab 23:84–89
Saxon LK, Turner CH (2005) Estrogen receptor β: the antimechanostat? Bone 36:185–192
Hatano H, Siegel H, Yamagiwa H, Bronk J, Turner R, Bolander M, Sarkar G (2004) Identification of estrogen-regulated genes during fracture healing, using DNA microarray. J Bone Miner Metab 22:224–235
Rodríguez J, Astudillo P, Ríos S, Pino A (2008) Involvement of adipogenic potential of human bone marrow mesenchymal stem cells (MSCs) in osteoporosis. Curr Stem Cell Res Ther 3:208–218
Yeung DKW, Griffith JF, Antonio GE, Lee FKH, Woo J, Leung PC (2005) Osteoporosis is associated with increased marrow fat content and decreased marrow fat unsaturation: a proton MR spectroscopy study. J Magn Reson Imaging 22:279–285
Acknowledgments
Financial support from the Fundação para a Ciência e Tecnologia (FCT), project PTDC/DES/103047/2008, is greatly acknowledged.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
Surgical craniotomy and graft implantation. a Exposure of the calvarial bone; b establishment of the standardized bicortical critical size calvarial defect; c graft implantation; d closure of the surgical wound (JPEG 101 kb)
ESM 2
Characterization of the osteoporotic conditions (n = 10). a Weight of Sham and Ovx animals throughout the healing period following craniotomy; b weight of the uteri from Sham and Ovx animals throughout the healing period following craniotomy; c representative 3D renderings of 6-month Sham animals, showing the analyzed volume of interest in the proximal tibia. Scale bar represents 1 mm; d representative 3D renderings of 6-month Ovx animals, showing the analyzed volume of interest in the proximal tibia. Scale bar represents 1 mm; e microstructural parameters of the trabecular structure of the proximal tibia in Sham and Ovx animals at the 6-month time point. Asterisk—significantly different from the Sham group (JPEG 84 kb)
Rights and permissions
About this article
Cite this article
Durão, S.F., Gomes, P.S., Colaço, B.J. et al. The biomaterial-mediated healing of critical size bone defects in the ovariectomized rat. Osteoporos Int 25, 1535–1545 (2014). https://doi.org/10.1007/s00198-014-2656-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2656-y